When it comes to medications, supplements, diets, and other trendy solutions for weight loss, if it sounds too good to be true, it probably is. And as anyone who knows me is aware, I am highly skeptical about quick-fix, one-size-fits-all treatments for any medical condition.
So, when I started to hear stories about Semaglutide (sold under the brand names Ozempic, Wegovy, and Rybelsus), my initial reaction was to wonder, “What’s the catch?” Could this medication, which was developed to treat insulin resistance really be as effective for weight loss as many people claim? And could it possibly be as safe as the pharmaceutical companies and the FDA have led people to believe it is?
Then, I started to recognize some patients who had struggled with losing weight, feeling healthier, and looking the best I had seen them in years! Seeing these amazing results with my own eyes forced me to take a deeper look into the Semaglutide craze that is taking over the weight loss industry.
In this post, I share what I discovered.
What Is Semaglutide?
Semaglutide is more than what you see on TikTok! It is an injectable medication that is typically prescribed in combination with diet and exercise to help control blood sugar levels in people with type 2 diabetes to manage weight.
Semaglutide works by mimicking the action of glucagon-like peptide 1 (GLP-1) — a naturally occurring hormone that has the following effects:
- Stimulates insulin production to help regulate blood sugar
- Inhibits glucagon release, slowing the release of sugar into the blood causing the body to burn more fat
- Slows gastric emptying to make you feel full longer
- Reduces appetite (because you feel full)
Together, these effects can help slow the conversion of sugar to fat, burn more fat, make you feel less hungry, and adhere to a healthy diet, all of which make it easier to manage weight and blood sugar.
Understanding the Connection Between Insulin Resistance and Weight
The research on diabetes, weight gain and loss, and inflammation is very clear — two thirds of all Americans are on a spectrum of insulin resistance. This means that their cells are not properly responding to the hormone insulin. What typically happens over time — and in response to a diet high in sugar — is that insulin receptors on cells become less responsive to insulin, which is why sugar is such a dangerous food!
As a result, even when your body is producing sufficient insulin, there may not be enough to stimulate the insulin receptors. When this happens, excess glucose is not properly metabolized, which can lead to weight gain, diabetes, heart disease, and more. If you struggle to lose weight, it’s likely due to poor sugar metabolism not necessarily caused by a lack of insulin.
Elevated blood sugar (or dysregulation of sugar metabolism) is the main culprit in type two diabetes, obesity, and weight loss resistance. Many people have elevated levels of blood sugar and are not considered diabetic. However, they cannot lose weight. Numerous diabetes medications act to combat elevated blood sugar and to some degree they work. However, where they often fall short is with respect to weight loss.
The combination of avoiding sugar and unhealthy fats, reducing portion sizes, and taking Semaglutide (Ozempic) as part of a medically prescribed and supervised plan of care may help reduce weight through better function of the insulin receptors. Patients using Semaglutide may find it easier to eat sensibly, due to diminished food cravings that result from better insulin secretion and reception.
How Semaglutide Works
Semaglutide works in several ways to help people more effectively manage their blood sugar levels and weight:
- Stimulates insulin secretion: Semaglutide functions like glucagon-like peptide 1 (GLP-1) — an incretin hormone — to stimulate GLP-1 receptors on cells. Incretin hormones are secreted in response to food intake. Every time we eat, our bodies are stimulated to secrete incretin hormones. GLP-1 is an incretin peptide hormone released from the lower digestive tract that, among other attributes, stimulates insulin secretion. In a similar manner, Semaglutide stimulates GLP-1 receptors, increasing insulin secretion, thereby reducing the amount of glucose in the bloodstream.
- Suppresses glucagon secretion: GLP-1 suppresses glucagon secretion and decreases hunger. Glucagon is a hormone released by the liver to increase the amount of glucose in the bloodstream. Slowing down the action of glucagon helps to keep blood sugar down.
- Reduces hunger: The higher your blood sugar is, the hungrier you feel. This is why when we eat cake, we want more! The combined effect of increasing insulin, decreasing glucagon, and slowing down gastric emptying leads to a feeling of satisfaction. This appears to be a great mechanism for weight loss especially when a person is weight loss resistant, diabetic, or obese.
Semaglutide and Liver Protection
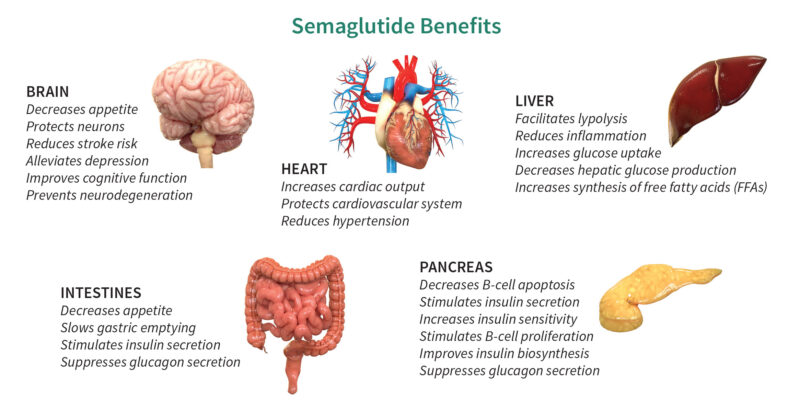
Additionally, Semaglutide has shown indirect protective action on the liver through the gut-pancreas-liver axis. That’s because it stimulates the breakdown of fat in the liver and reduces glucose production by the liver, thereby improving insulin resistance. Semaglutide, as with other peptides (molecules that contain two or more amino acids), has multiple beneficial downstream effects since there are receptors for GLP-1 throughout the body including in the brain, liver, pancreas, peripheral nervous system, gastrointestinal tract, cardiovascular system, kidneys, and lungs.
Having normal insulin physiology is also important for the prevention of many chronic conditions, including diabetes, kidney disease, liver disease, heart disease, and neurodegenerative diseases such as Parkinson’s, Alzheimer’s, and dementia.
Semaglutide Benefits
If you are struggling to lose weight (or not gain weight) or you have been diagnosed with type-2 diabetes, insulin resistance, or slow metabolism, Semaglutide may be a valuable component of your medically supervised treatment plan. Although Semaglutide’s primary benefits are related to weight loss and regulating blood sugar, it has a long list of potential benefits, including the following:
- Slows gastric emptying, which can lessen appetite, making it easier to eat less
- Lasts a relatively long time — can be taken once a week
- Is selectively active when food is consumed, therefore, even though it lowers blood sugar, those with hypoglycemia (low blood sugar) are not negatively impacted
- Increases the sensitivity of the insulin receptors, thereby reducing the burden on the pancreas while lowering blood sugar — a hallmark of weight loss
- Helps the body to both produce and release insulin in the presence of food
- Strengthens the beta cells of the pancreas, thereby reducing programmed cell death to the beta cells of the pancreas which produce insulin
- Supports the body’s ability to produce insulin rather than supplementing with insulin medication (the traditional approach to treating diabetes)
- Appears to have cardiovascular benefits
- Has beneficial effects on the brain, heart, pancreas, and liver
- Affects satiety, water intake, stress reaction, neurogenesis, neurodegeneration, thermogenesis, and energy homeostasis
Case Study
Several months ago, I added Semaglutide to a patient’s plan of care. This patient had been struggling with weight loss for their entire life and, at 45 years old, was unable to lose weight despite their best efforts over the past decade. I’ve seen this situation many times throughout my years in practice.
Normally, changing a patient’s diet to an anti-inflammatory diet and adding some supplements to promote weight loss and improve insulin resistance can make a big difference. However, this patient had tried everything, including low-fat and keto diets, B12 injections, phentermine, and more. Additionally, they had a variety of other symptoms, such as chronic fatigue, constipation, heartburn, allergies, joint pain, migraines, and restless sleep.
After six months of treatment, all of their symptoms, including fatigue, improved, except for their weight. I often wondered how this could happen and postulated that something was happening at the receptor level impacting insulin, since their glucose and insulin labs were normal. However, after three months on Semaglutide, they lost over 30 pounds and were ecstatic! Our appointments and conversations remain focused on keeping their weight down to reduce the risk of chronic conditions, such as heart disease. It’s important to note that Semaglutide can be used as a tool but building the right infrastructure for long-term results is crucial. When done properly, it’s a beautiful thing to see a patient achieve a goal they’ve been working on for decades.
Potential Adverse Side Effects
Semaglutide is a relatively safe medication. However, side effects may include:
- Nausea
- Constipation
- Decreased appetite (which is one of the benefits, as well)
- Dizziness
- Hypoglycemia
- Vomiting
- Abdominal pain
- Diarrhea
- Headache
- Fatigue
- Increased lipase
- Acid reflux
- “Ozempic face,” which is the loss of facial fat that can make the face look gaunt or droopy due to rapid weight loss
The most common adverse side effects are related to digestion and its incretin functions. These side effects may be due in part to slower gastric emptying time and lowered blood sugar leading to hypoglycemia.
Risks of these side effects can be reduced by using the lowest effective dose and gradually increasing the dose over several weeks. Additionally, injections of B vitamins have been found to be helpful in reducing any nausea resulting from treatment with Semaglutide.
Other less common side effects include the following:
- Malaise
- Pancreatitis
- Rapid heart rate
- Urticaria (hives)
The Bottom Line on Semaglutide (Ozempic)
So, to answer the question I posed at the beginning of this post, Semaglutide is not too good to be true. It’s safe and effective for treating type 2 diabetes and for long-term weight management, especially when used in combination with diet and exercise. (Note that Semaglutide is not a replacement for insulin. If your pancreas isn’t producing insulin, you will need to continue taking insulin.)
If you’ve tried everything to lose weight and have had little to no success, I strongly recommend discussing the possibility of adding Semaglutide to your personalized plan of care with your healthcare provider.
– – – – – – –
About the Author: Dr. Matt Lewis, D.C., DACBN, CFMP®, specializes in diagnosing and treating the underlying causes of the symptoms related to chronic and unexplained illness through nutrition, lifestyle, chiropractic, and other natural approaches to whole-health healing in Tampa, Fla. Dr. Lewis has 20 years of experience practicing nutritional and holistic medicine. He earned his B.S. in Biology from Shenandoah University, his Doctorate in Chiropractic from Life University, his Diplomate status in Clinical Nutrition from the American Clinical Board of Nutrition, his CFMP® from Functional Medicine University, and his certification as a Digestive Health Specialist (DHS) through the Food Enzyme Institute. Dr. Lewis’ passion for health and wellness stems from his own personal experience. With a family history of autoimmune conditions and diabetes, and his own lab tests showing his genetic susceptibility to Hashimoto’s thyroiditis (autoimmune thyroid), he has learned how to restore his own health and vigor to prevent the onset of these and other illnesses and live an incredibly active life. Through this process, he acquired a deeper understanding of health and wellness, which he now offers his patients in Tampa and elsewhere.



Thank Matt, I will be talking to my Doctor next month as this sounds like an option that might help me out.
We appreciate you sharing your research and stating that semaglutide has demonstrated indirect liver protection through the gut-pancreas-liver axis. You claimed that this improves insulin resistance by encouraging the liver’s fat breakdown and reducing the liver’s synthesis of glucose. My buddy has struggled with obesity her entire life and wants to lose it so she may regain her confidence. I’ll let her know about semaglutide and share this with her. Thanks.
Wow, I had no idea that semaglutide help you lose weight by affecting blood sugar. I’ve been unable to lose weight for about three years, and I’m getting really discouraged about it. It’d be good to talk to my doctor to see if semaglutide would help me at all.