At some point in our lives, most of us can expect to experience some form of anxiety. It might occur as the result of a life challenge, whether that be a relationship, health issue, work conflict, finance, or traumatic event. Such anxieties are normal and seldom anticipated.
Having said that, I believe it’s important to avoid downplaying the impact that stress has on our lives. It can ruin a person’s health and yet it’s so often treated superficially or worse — it’s blown off by the medical provider.
However, if you are going through a period of acute stress, or you remain in a state of chronic stress and now find yourself feeling fatigued, unmotivated, or irritable, you may be experiencing the negative health impacts of stress. And that stress might possibly be diagnosed as Generalized Anxiety Disorder (GAD).

In our culture — curated as it is by conventional medicine — anxiety is often seen as a disorder and, in such fashion, labeled GAD. However, anxiety is also a normal part of life. It’s a normal part of physiology and in many cases it’s not a disorder. When anxiety becomes a disorder, it is far more obvious to recognize in ourselves and those around us and there is a greater likelihood a diagnosis of GAD will be provided by a psychologist or similar health care professional.
Whether you actually have GAD or just suffer mild to moderate anxiety, it can feel as if you’re being treated for anxiety or depression abstractly, and even with such treatment your health can decline because the underlying issues have not been resolved.
I have observed many patients seeking out functional medicine or holistic medicine who are struggling with a low to moderate anxiety level that doesn’t fit the formal diagnosis of Generalized Anxiety Disorder.
Some men and women can be reluctant in acknowledging their anxiety, while others freely discuss their concerns. It is also common for people to dismiss anxiety or lower the value it has on their health outcomes. In some ways I think we have the wrong understanding of what anxiety is and how it blocks us from reaching our optimal health.
Breaking anxiety down, I like to classify it as follows:
- Generalized Anxiety Disorder — advanced anxiety often benefitting from prescription medication
- Moderate/ mild anxiety — successfully treated without the use of prescription medication
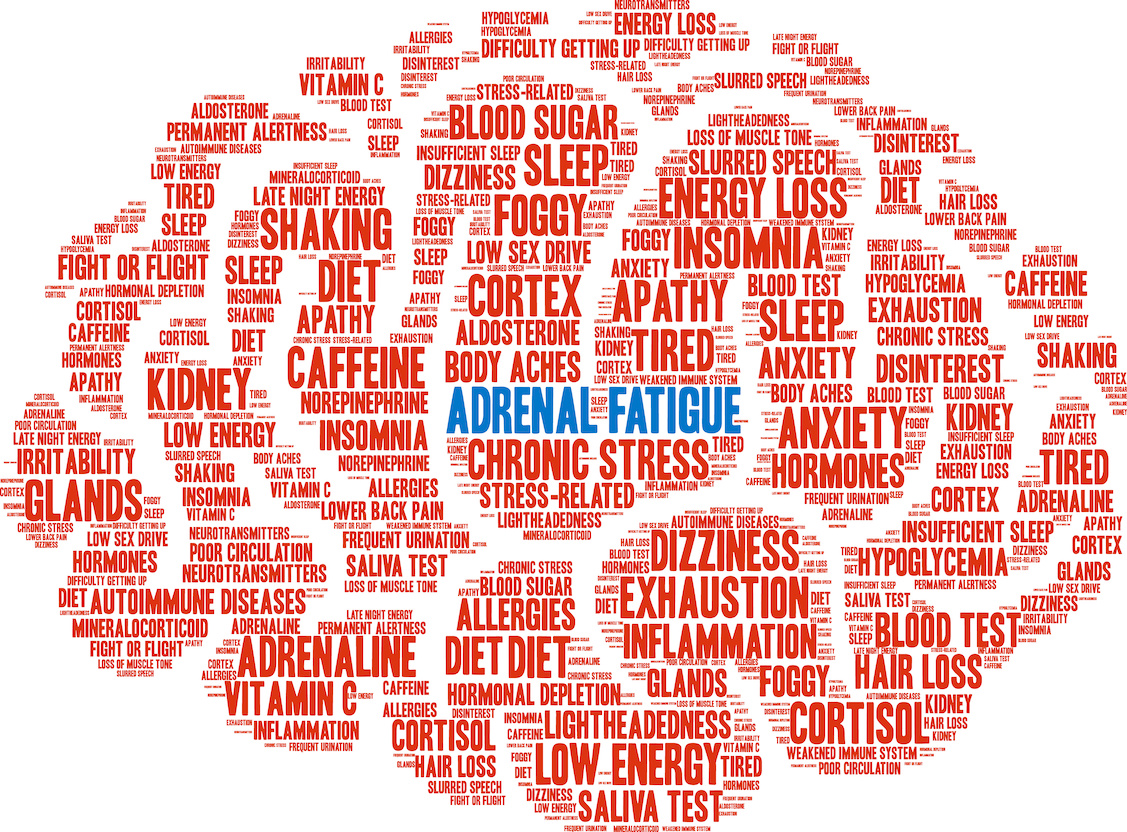
Conditions and Symptoms Associated with GAD and Moderate to Mild Anxiety
Anxiety can create or exacerbate many conditions including:
- Chronic Fatigue
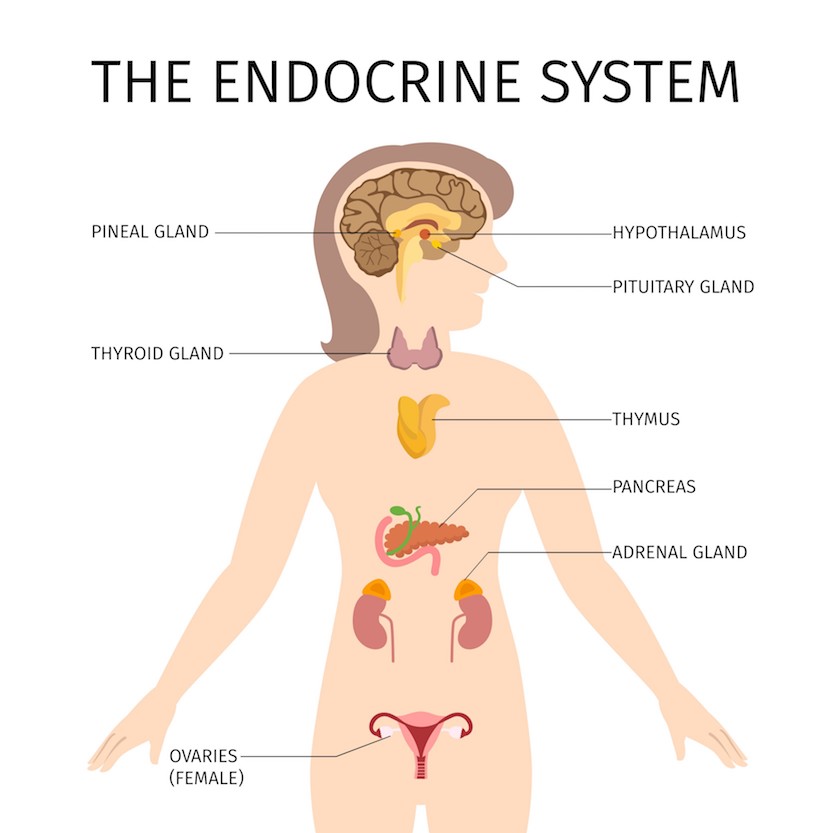
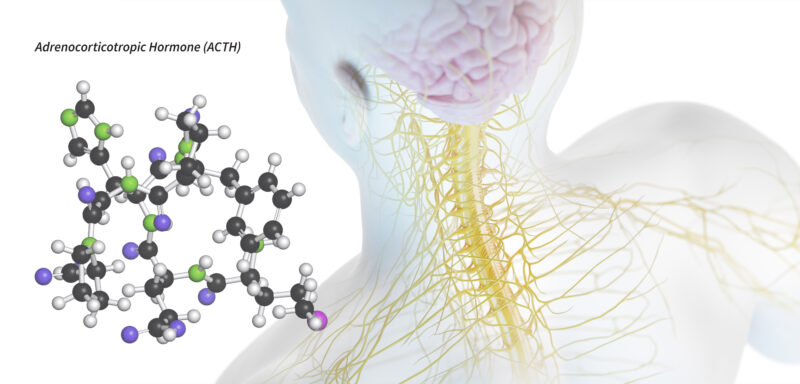
- Cortisol Imbalances
- Hormone Imbalance, altered libido or painful cycles
- Hypoglycemia
- Irritable Bowel Syndrome (IBS) — Constipation or Diarrhea
- Insomnia or restless sleep
- Neurological Symptoms
- Restless Legs
- Weight Gain or Loss
Besides the commonly known symptoms of anxiety, which cause worry, upset and inability to relax, there are others, including: Continue reading…