Welcome to the Blog of
Dr. Matthew Lewis
Here, you’ll find news from our office, insights and observations from trusted sources in health, information about innovations in the effort to take back your own good health, testimonials from our clients, resources and recommendations of note, and more. Read a post or two and comment on anything that strikes a chord.

Florida is No. 1 in The Nation for Mold — Here’s How to Protect Your Family
Florida leads the nation in a number of things, including being the most favored destination for people who are retiring. It’s also the most popular state for new business formations —outside of Delaware, which is a business formation mill. And the Sunshine State is also No. 1 for something called Education Freedom, which enables students and parents a choice of educational options that best meet their needs.
We could go on and on with these “best in the nation” accolades, but this post deals with what we consider one of Florida’s least laudable attributes: mold. Hands down, Florida is No. 1 in nation in mold.

According to a March 2024 study, Florida scored 38.76 out of a possible 40 on the FDP Mold Index. Mississippi ran a close second at 38.66 and Louisiana came in third with 38.52. FDP’s mold index is based on four key metrics that can be attributed to higher chances of mold growing inside and outside the home:
- Average rainfall
- Average temperature
- Average humidity
- Average age of homes
Each metric accounts for 10 of the total 40 points.
These scores are no surprise to our medical team here at PROVOKE Health. Many of our patients live in Tampa and other areas in South Central Florida, and their initial visit to our clinic or via a virtual appointment is often because they’re seeking relief from symptoms commonly related to mold exposure. These patients typically have already consulted with conventional medical practices without receiving much, if any, relief. Some of these medical practices don’t even offer a clear diagnosis.
At PROVOKE Health, we provide relief through a highly personalized protocol that addresses everything from in-home testing and mold remediation to blood draws, detoxing, and treating any mold/fungal infection. We calm the inflammatory response and restore health and function to the body’s nervous system, which is often impacted by mold exposure. And while we don’t test homes or perform mold remediation ourselves, we have a list of trusted companies that do as part of our treatment protocol.
Recognizing the Symptoms of Toxic Mold Exposure
Mold exposure can cause infections, especially sinus infections, as well as overwhelm the body’s natural detox mechanisms. Infections and toxins can cause chronic inflammation, which produce symptoms that are vague and difficult to trace back to a clear underlying cause unless you’re a trained medical professional who knows what to look for. Symptoms of mold exposure include, but are not limited to, the following:
The Power of Peptides in Reducing Brain Inflammation
Marilyn, an otherwise healthy 45-year-old woman, first visited our functional medicine and integrative healthcare clinic complaining of unrelenting fatigue, brain fog, loss of concentration, difficulty recalling words, and restless sleep.
She had seen other doctors, and they were unable to offer a diagnosis or any effective treatments. Her brain MRI scans came back as normal, and the neurologists with whom she consulted found no notable dementia or neurological disease that could explain her symptoms.
Her nervous system and brain were seemingly intact. All good from the perspective of conventional medicine, but Marilyn knew better; clearly, her brain was not functioning optimally. Marilyn’s symptoms were classic signs of brain inflammation. We had seen these same symptoms in hundreds of patients in the past. We knew the causes, and we had effective treatments to help her.
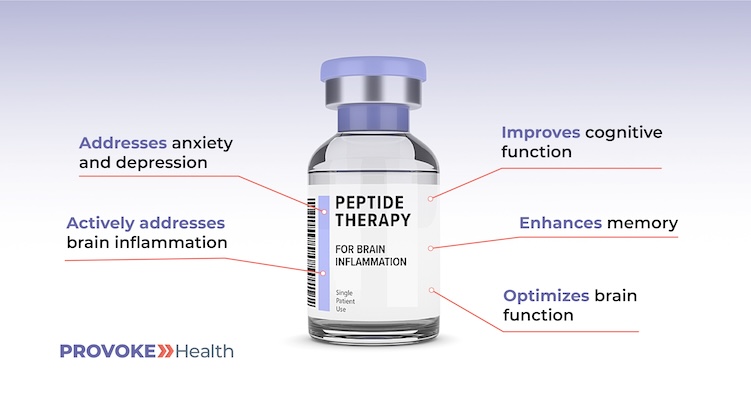
In this post, we look at common causes of brain inflammation and the PROVOKE Health approach to treatment, which may include the use of medically prescribed therapeutic peptides such as:
- Semax
- Selank
- Thymosin Beta 4
Exploring the Causes of Brain Inflammation
In Marilyn’s case many of the common symptoms of brain inflammation were there: exhaustion, clouded thinking and brain fog, poor sleep, anxiety, and a steep decline in quality of life. But before I (Dr. Lewis) go deeper into the specifics of Marilyn’s case, let’s take a look at the bigger picture.
Other Health Conditions Linked to Brain Inflammation
Numerous health conditions can negatively impact brain health and function, including the following:
Weight Loss Benefits — and Side Effects — of Semaglutide and Ozempic
In recent years, medical researchers and pharmaceutical companies have made remarkable progress in the area of diabetes management. Specifically, semaglutide (sold under the brand names Ozempic, Wegovy, Rybelsus, and others) has proven to be effective in helping people with Type 2 diabetes regulate their blood glucose (sugar) levels.
As an added bonus, semaglutide has also proven to be effective in promoting weight loss for many people. Likely you’ve heard or read all about that by now. And you certainly wouldn’t be the first to wonder if semaglutide could work that magic on you.
Here at PROVOKE Health, we too have observed some amazing results in our functional medicine and integrative health clinic, with people who have struggled for years to lose weight suddenly shedding pounds, feeling great, and looking better than they had in years.
However, recent reports of adverse side effects have begun to emerge — side effects such as nausea, diarrhea, vomiting, constipation, abdominal pain, fatigue, malnutrition, and “Ozempic face” (the rapid loss of facial fat, which can make the face look gaunt or droopy).

In this blog post, we review some of the arguments for and against semaglutide. But first, let’s take a look at what this medication is, how it works (its mechanism of action), and some of its common adverse side effects.
What Is Semaglutide?
Semaglutide is the generic name for a group of antidiabetic medications classified as glucagon-like peptide-1 receptor (GLP-1R) agonists. Some GLP-1R agonists, including Ozempic, can also be very effective in promoting weight loss and treating obesity. (For more about this, read our previous blog post, “Ozempic for Weight Loss: Too Good to Be True or an Effective Treatment,” here on the PROVOKE Health blog.)
Most of the medications in this class are injectable, meaning you inject a liquid form of the medication using a needle and syringe. Injections are delivered to the fatty tissues beneath the skin in certain areas of the body, including the belly, outer thighs, and upper buttocks.
Semaglutide has earned a great deal of positive press for its promising benefits, especially in respect to weight loss. However, like any medication, this class of medications carries potentially negative side effects. Prior to taking semaglutide or any of its brand-name equivalents, it is important to weigh the potential benefits against the possible adverse side effects before adding these medications to your diabetes management or weight loss plan.
How Semaglutide Works
Two thirds of people in the United States suffer, to some degree, from insulin resistance. That means their cells don’t respond properly to insulin — a hormone the body produces to stimulate the metabolism of sugar. Over time, the insulin receptors on cells become less and less responsive to insulin, especially when subjected to a high-sugar
We’re Now Offering IV Nutrient Therapy in Tampa, Florida
PROVOKE Health (formally Functional Healthcare Group, and still Dr. Matt Lewis’ healthcare practice) is now offering medically supervised IV nutrient therapy for its patients and select walk-ins in Tampa / South Central Florida. But what does that mean exactly? Let’s unpack that statement to find out.
Functional medicine is a patient-centered healthcare model that seeks to identify and treat the root cause(s) of chronic illness all the way down to the cellular level. Medically supervised IV nutrient therapy delivers vitamins, minerals, and other nutrients directly through the bloodstream to cells throughout the body to optimize their health and function.

Delivering nutrients via IV drip allows them to travel directly to the cells so that nothing is lost in the digestive process. As a result, your body gets more nutrients faster.
By improving and then leveraging your body’s natural ability to fend off illness and repair health, we’re able to successfully treat a variety of health conditions that other doctors’ offices choose to ignore, don’t test for, or don’t know how to treat. IV nutrient therapy, when incorporated into a handcrafted plan of care, plays a key role in restoring health by providing the body the essential micronutrients it requires for optimal function.
When you’re grappling with acute or chronic illness, the efficiency of a nutrient-packed IV may turbocharge the healing process. By directly targeting the affected cells with a concentrated blend that addresses your specific needs, we jumpstart the healing process, enabling your body to respond promptly to treatment. Each IV is carefully formulated to address your health history, symptoms, and desired health and fitness objectives.
Our IV Nutrient Therapies
Currently, we are offering the following IV nutrient therapies:
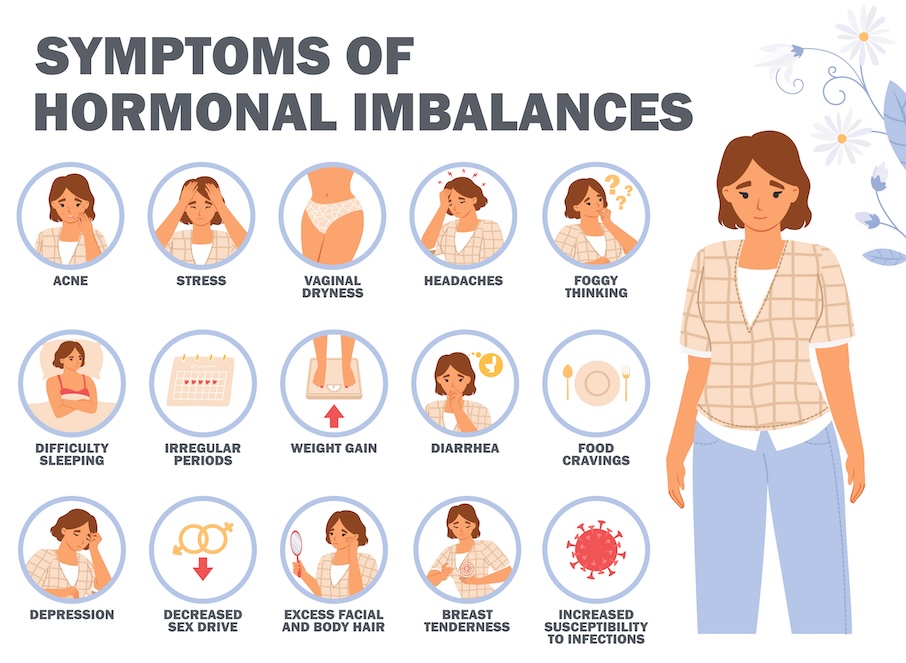
Feeling Your Best During Perimenopause and Beyond
Despite popular narratives, perimenopause isn’t just about hot flashes, night sweats, sex hormones, ovulation, and the natural transition to menopause. It extends beyond hormones to impact muscle mass, bone density, cardiovascular health, cognitive function, mood, skin health, sex, and more.
Perimenopause of course is a natural phase before menopause when a woman’s body starts shifting, causing irregular periods, mood swings, and other changes due to fluctuating hormone levels, marking the transition to the end of reproductive years. It’s like a rollercoaster ride for the body, with ups and downs, as it prepares for the next stage of life.
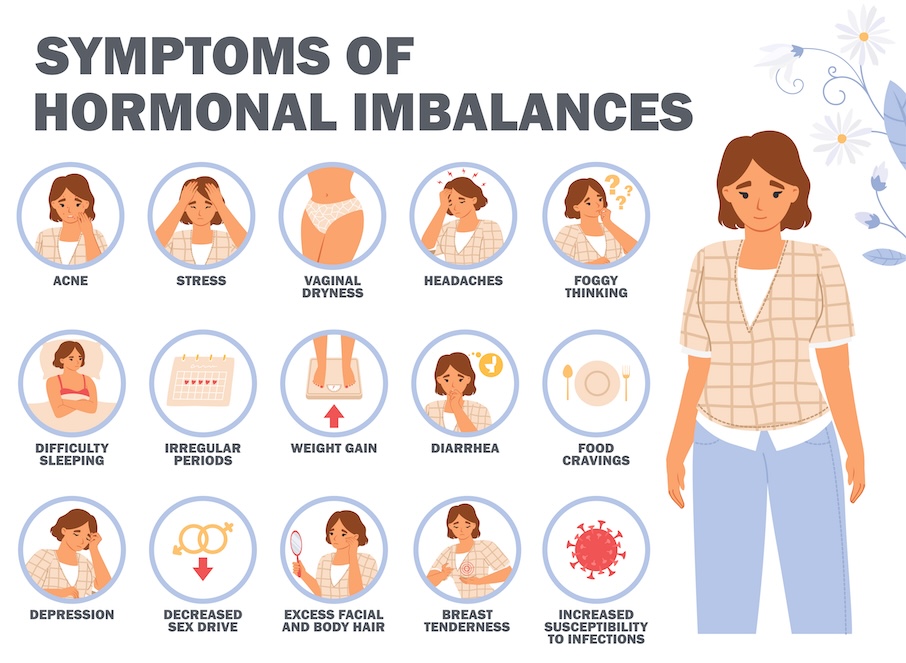
In this post, I call attention to how low estrogen caused by perimenopause can negatively impact your health, and what you can do to slow and even reverse the progression of health conditions related to declining estrogen.
Addressing Muscle Loss
Muscle loss for women typically begins in one’s 30s or 40s and becomes more pronounced with aging. It’s a gradual process, and its progression can vary among individuals in response to numerous factors, including the person’s health history, genetics, exercise regimen, diet, and stress. A decline in estrogen levels during menopause (usually occurring in the late 40s or 50s) can contribute to the acceleration of muscle loss in women.
One important aspect of healthy aging is to avoid the loss of muscle mass or, even better, build muscle mass as you age. This is entirely possible to accomplish with the right combination of hormone replacement therapy (HRT), exercise, proper diet, and medication to stimulate growth hormone.
It’s no secret that as we age, we tend to lose muscle mass, but muscle is more than what meets the eye. It has a range of impacts on the body, including functional strength and independence, metabolic and hormonal health, bone health and prevention of chronic disease. Here are a few ways that muscle health impacts overall health:
Diagnosing and Treating Multiple Chemical Sensitivity (MCS)
Some medical conditions are relatively easy to diagnose with a standard blood test, urine test, or medical imaging. Among them are diabetes, anemia, impaired kidney or liver function, certain thyroid disorders, and certain infections and cancers.
However, Multiple Chemical Sensitivity (MCS) isn’t one of those conditions. In order to diagnose MCS, doctors must first be aware of the condition, and then generally must rely on a clinical diagnosis — a trained doctor’s best guess based on the signs and symptoms of the illness and the patient’s medical history, rather than on lab tests or medical imaging.

That’s a problem, because most conventional doctors have trouble accepting that multiple chemical sensitivity is a bona fide illness, and without hard evidence, such as that provided by lab tests or medical imaging, patients can’t prove that they have a medical condition. I often see patients who have been suffering with MCS for years on end. They’ve been to a half dozen doctors or more who’ve been unable to offer any explanation for their symptoms. In some cases, their doctors have gone so far as to suggest that nothing is medically wrong with them, or even led them to believe that “it’s all in your head.”
I’m here to tell you that if you’re experiencing symptoms of multiple chemical sensitivity — which I will describe in this post — you have a real medical condition. It’s certainly not a figment of your imagination, and you’re not a hypochondriac. I’m also here to tell you that bona fide medical treatments are available to alleviate your symptoms and put you back on the road to recovery.
Understanding Multiple Chemical Sensitivity
Multiple chemical sensitivity (MCS) is a medical condition that causes a person to react to low levels of certain chemicals in their environment, such as the following:
- Cleaning products
- Detergents
- Off-gassing from furniture or building materials
- Paint
- Perfumes and other fragrances
- Pesticides
- Plastics
- Tobacco smoke
- Vehicle exhaust fumes
Electromagnetic fields may also pose a risk to some individuals.
While most people without MCS tolerate low levels of these chemicals, people with MCS react to them. It’s not technically an allergic reaction, but it can trigger allergy-like symptoms that cause discomfort or negatively impact your quality of life.
Recognizing the Signs and Symptoms of Multiple Chemical Sensitivity
Multiple chemical sensitivity symptoms differ among individuals who have the condition, but generally include one or more of the following:
Diagnosing and Treating Mast Cell Activation Syndrome (MCAS)
Mast cell activation syndrome (MCAS) is a complex and often misunderstood disorder of the immune system that occurs when mast cells — a type of white blood cell — trigger an excessive inflammatory response.
MCAS can cause a range of symptoms, including skin rashes, itching, flushing, bloating, constipation or diarrhea, difficulty breathing, fatigue, headaches, joint and muscle pain, and neurological symptoms. It often makes people hypersensitive to foods they never had a problem eating in the past.
Based on their symptoms, patients with MCAS are often diagnosed as having allergies, asthma, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), postural tachycardia syndrome (POTS), an inflammatory bowel disease (such as Crohn’s or ulcerative colitis), or another medical condition. Meanwhile, their underlying MCAS, which is the root cause of their symptoms, remains undiagnosed and untreated.
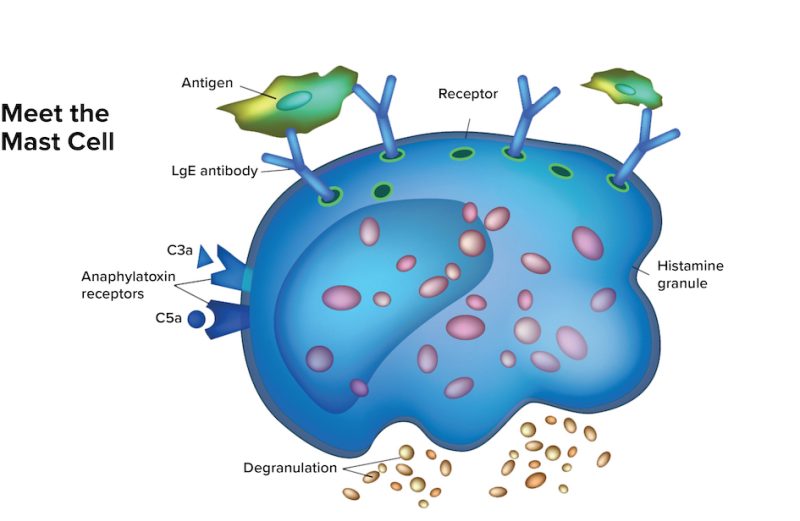
If you’re experiencing the symptoms I described or you’ve been diagnosed as having one of the conditions I mentioned, you’ve probably been prescribed medication to alleviate your symptoms. Medication for symptom relief may be effective to some degree for a period of time, but it doesn’t fully address the underlying issue. As a result, you’re likely to continue to suffer.
Through this post, I’m hoping to increase awareness of mast cell activation syndrome, so more patients can get the right diagnosis and effective treatment.
Identifying Your Triggers
When they function properly, your mast cells play an important role in protecting your body against pathogens, such as infectious bacteria and viruses. When these cells perceive a potential threat, they release chemical mediators — including histamine — to launch a rapid immune response intended to destroy and eliminate the pathogen.
However, when these cells become overly sensitive, they release chemical mediators in response to non-threatening triggers. Sometimes, they release too much. Triggers vary among individuals and may include the following:
Is a B12 Deficiency Making You Sick?
B12 deficiency can sneak up on you. You’re feeling strong and energetic, thinking clearly, feeling upbeat, and then gradually, maybe over the course of several months or even years, you begin to notice that you’ve lost the pep in your step.
Your mind and memory aren’t as sharp as they once were. Even mildly strenuous physical activity leaves you breathing hard, and instead of feeling pumped up after exercise, you feel exhausted.
What happened?
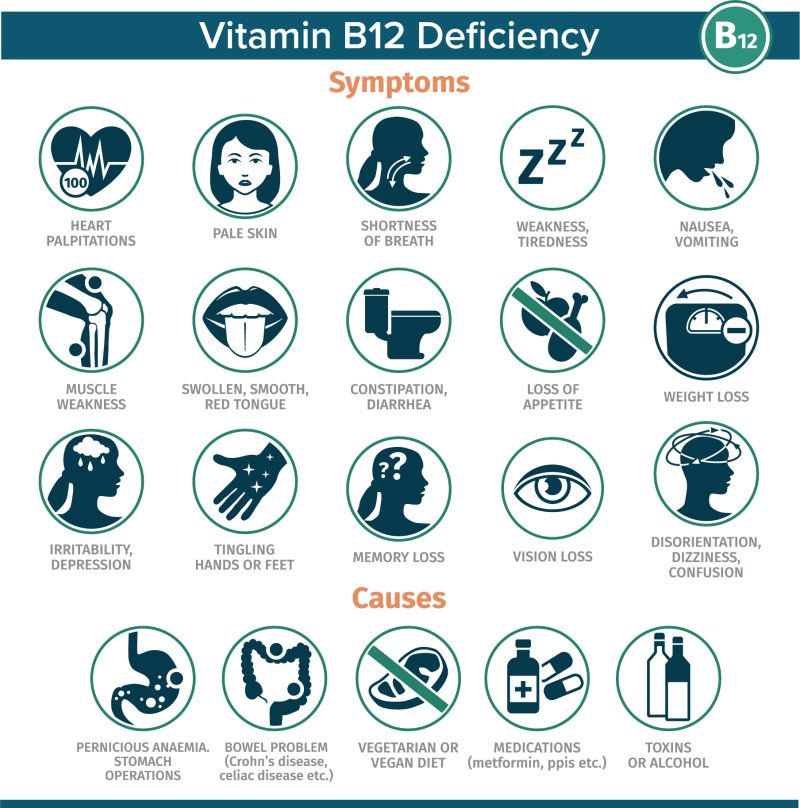
Without a thorough workup, complete with analysis of targeted lab tests, you’ll never know what’s causing you to feel rundown. It could be stress, a lack of (or too much) exercise, a buildup of environmental toxins, or an undiagnosed infection. Or it might be any number of nutritional deficiencies, a combination of those deficiencies, or countless other possible contributing factors.
That’s why I always recommend consulting with a healthcare professional who is attached to a functional medicine practice and obtaining a complete workup and personalized plan of care before starting any treatment, or even taking an over-the-counter supplement. Until you test, you don’t know the root cause of what’s ailing you or what your body may be lacking.
A complete workup often reveals numerous contributing factors and root causes, and one common factor is a vitamin B12 deficiency. Unfortunately, diagnosing and treating B12 deficiency and its underlying cause(s) is more complicated than just ordering a blood test and taking a B12 supplement. In this post, I explain why. But first, it’s important to recognize the symptoms and possible causes of B12 deficiency.
Symptoms of Vitamin B12 Deficiency
Vitamin B12 plays an important role in physiological processes that affect different systems in the body. As a result, symptoms of B12 deficiency can vary considerably, both in symptom type and severity. Here are some common symptoms associated with B12 deficiency:
- Fatigue and weakness: Feeling unusually tired and weak is one of the most common symptoms of B12 deficiency. This is because B12 is essential for the production of red blood cells, which carry oxygen throughout the body.
- Anemia: B12 deficiency can lead to a type of anemia called megaloblastic anemia. In this condition, red blood cells are larger and fewer in number, which can result in reduced oxygen-carrying capacity and lead to fatigue, pale skin, and shortness of breath.
- Nervous system dysfunction: B12 plays a crucial role in maintaining the health of the nervous system. Deficiency can lead to symptoms such as numbness, tingling, or a “pins and needles” sensation in the hands and feet. It can also cause difficulty walking, balance problems, and even affect cognitive functions including memory and concentration.
- Neuropsychiatric symptoms: B12 deficiency has been associated with mood changes, including depression, anxiety, and irritability. Some individuals may experience more severe
Benefits of Boosting Human Growth Hormone (HGH) for Recovery and Resilience
For many of us, as children and teenagers and even into our 30s, we found ourselves strong and energetic, recovering quickly after moderate and even intense exercise, and often immune to daily aches and pains. As we aged beyond those years, however, we started to lose our stamina and ability to quickly recover.
More and more exercise is required just to maintain our strength, flexibility, and vitality. It takes longer for us to recover from those exercise sessions, and we’re more susceptible to injury. Why is this? What do we lack in our later years that we had in abundance in our youth?

The answer is human growth hormone (HGH). HGH stimulates and regulates the growth and lifecycle of nearly every cell in the body. And when you reach the age of about 30 years, your pituitary gland releases less and less HGH with each passing year. This decline can occur rapidly, and to be clear, it is a normal part of aging. However, this reduction of HGH is largely responsible for many of the signs associated with aging:
- Lower energy
- Decreased muscle mass and inability to build new muscle
- Increased difficulty losing or maintaining weight
- Weakened immune system
- Decreased healing efficiency
- Other signs of physical and mental aging
Today, I want you to know that by working with functional medicine-focused doctor, you can work on reversing this process and boost HGH in two ways:
- Directly via injections of synthetic human growth hormone, which is typically recommended only for people whose pituitary gland is damaged or dysfunctional
- Indirectly by stimulating the pituitary gland to release more human growth hormone that your body produces naturally
Stimulating the Pituitary Gland to Release More HGH Naturally
Stimulating the pituitary gland to release more human growth hormone is the safer way to increase HGH, and there are several ways to do it:
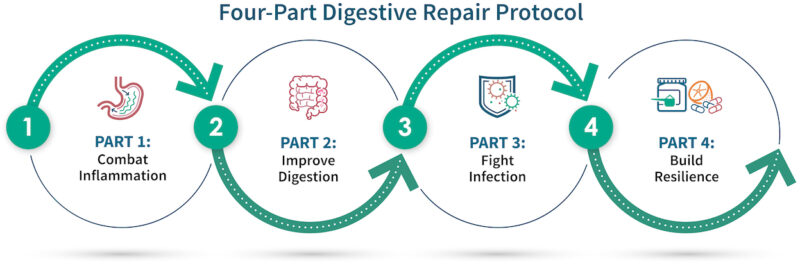
Restoring Gastrointestinal Health and Function: Part Two — Testing and Treatment
Welcome Part Two in my series on gastrointestinal (gut) health and function. In Part One, I covered several ways that the gut supports overall health, explained common factors that can impair gut health and function, and described obvious and not-so-obvious symptoms that can arise when gut health is compromised. In this part, I turn my focus to testing for gut dysfunction and restoring and optimizing gut health and function.
Testing to Rule Out or Confirm and Identify Gut Issues
Based on our initial consultation and examination, I may suspect that the health issues you are experiencing are related to your digestive system. However, testing is required to confirm any suspicion I may have (or rule it out) and to identify more precisely what is going on. If I suspect that gut dysfunction may be at the root of your symptoms, I will recommend one or more of the following tests:
- GI Map Stool: This comprehensive study of bacteria, viruses, parasites, and digestive function checks for leaky gut, inflammatory bowel disease, gluten sensitivity, blood loss, and pancreatic enzymes.
- Microbial Organic Acids Test (MOAT): This urine test checks for overgrowth of potentially harmful bacteria and yeasts, levels of beneficial bacteria, and metabolic issues. Organic acids are metabolic intermediates involved in several processes, including energy production, detoxification, and the breakdown of neurotransmitters. Levels of specific organic acids serve as valuable indicators of digestive function.
- SIBO Breath Test: This test measures gases produced by bacteria in the small intestine. Results can help identify a bacterial overgrowth.
- Abdominal/Liver Sonogram: This exam is often used to check for fatty liver, which can disrupt metabolism and detoxification pathways. Results reveal any signs of inflammation or indications of any blockage of bile flow from the gallbladder. Based on the results, I may refer you to a gastroenterologist for an endoscopy or colonoscopy and follow-up treatment.
- Pelvic Sonogram: This exam may reveal uterine fibroids or cysts that can cause abdominal discomfort, pain, and altered digestion. If I think a transvaginal sonogram is required, I will refer you to a gynecologist.
I may also recommend the elimination of certain inflammatory foods from the diet, such as dairy, sugary foods or beverages, alcohol, fried foods, or refined carbohydrates to determine whether certain foods or classes of foods trigger or worsen symptoms.
Targeting the Three Factors That Impact Gut Health and Function
Gut health is complex but can best be understood by examining the following three factors that play a pivotal role in gut health and function:





Recent Comments