Do you suffer from bloating, gas, or chronic diarrhea? Have you been diagnosed with irritable bowel syndrome (IBS)? If so, the problem may not be your gastrointestinal tract but what’s inside it. You may have SIBO.
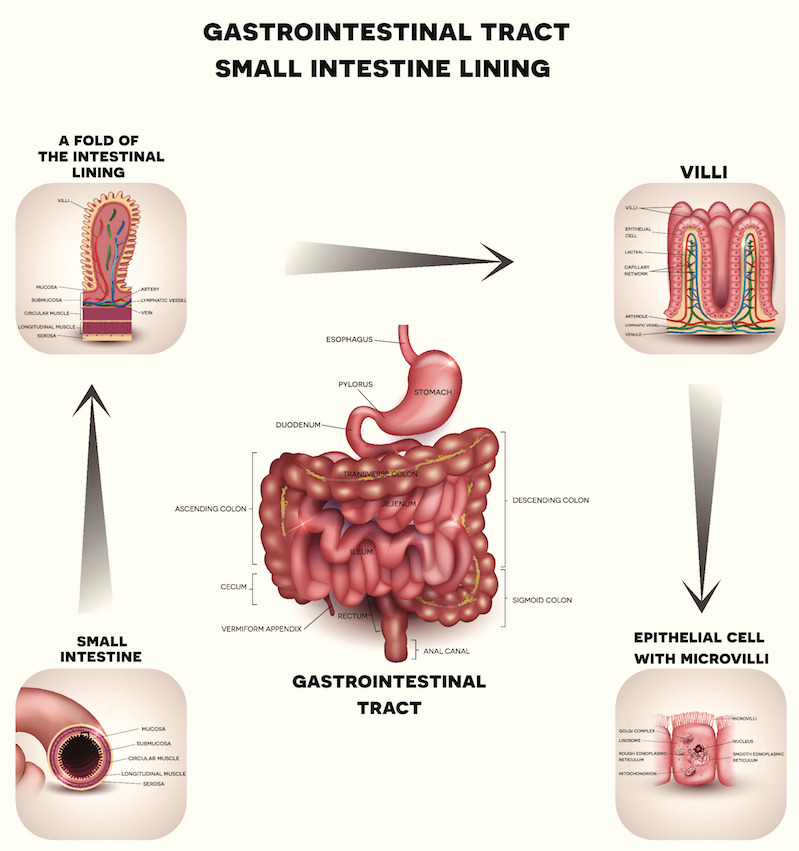
SIBO is short for small intestinal bacterial overgrowth — the presence of excessive bacteria in the small intestine and/or changes in the types of bacteria normally present. (The small intestine, or small bowel, is the section of the gastrointestinal tract that connects the stomach to the large intestine and is responsible for most nutrient absorption.) SIBO is often the underlying cause of chronic diarrhea, nutritional deficiencies, unplanned weight loss, and osteoporosis.
Left untreated, SIBO negatively impacts the structure and function of the small intestine. The overpopulation of bacteria can damage the lining of the small intestine, which can cause leaky gut — a condition in which large protein molecules pass through the intestine into the bloodstream, triggering immune reactions that can result in food allergies or sensitivities, chronic inflammation, and autoimmune diseases.
Recognizing the Risk Factors
The following risk factors increase the likelihood of a person developing SIBO:
- Low stomach acid, often due to the overuse of antacids or a condition called hypochlorhydria, in which the stomach produces insufficient stomach acid
- Overuse of antibiotics, which can lead to an imbalance of microorganisms in the small intestine
- Irritable bowel syndrome (IBS), which is typically caused by SIBO or by an inflammatory bowel disease (IBD) such as Crohn’s
- Diverticulitis — a condition in which small, bulging pouches develop in the digestive tract
- Long-term celiac disease (gluten intolerance)
- Metabolic disorders, including diabetes
- Gastroparesis — a condition that affects the stomach muscles or nerves, inhibiting proper muscle function, which results in the inadequate grinding of food and the impaired emptying of the stomach contents into the small intestine
- Organ system dysfunction, including cirrhosis, renal failure, and pancreatitis
Diagnosing SIBO and Its Underlying Causes
SIBO is easy to diagnose through the use of non-invasive hydrogen and methane breath testing. During the test, you drink a small amount of test sugar and then blow air into a bag at regular intervals. Tests results indicate whether you have SIBO.
I also perform the following tests:
- Blood tests for vitamin and mineral levels: SIBO can affect vitamin and mineral levels in two ways. First, if SIBO damages the lining of the small intestine, it can inhibit the absorption of nutrients from food. Second, bacteria in the gut produce many vitamins; if certain vitamin producing bacteria are crowded out by other bacteria, low levels of that vitamin will result. As gut health and function are restored, we supplement with vitamins and minerals to ensure that all cells in the body are receiving proper nutrition.
- Physical exam to assess Vagus Nerve function: A weak gag reflex is an indication that Vagus Nerve function is impaired. The Vagus Nerve stimulates the stomach muscles. If the nerve isn’t signaling the stomach muscles to contract, motility issues arise. (Motility refers to the muscle contractions that mix and propel the contents of the stomach through the gastrointestinal tract.) Any Vagus Nerve function impairment must be addressed.
- Gastrointestinal Microbial Assay Plus (GI MAP) stool testing: This non-invasive stool test uses DNA technology to identify parasites, bacteria, and viruses and asses overall digestive function. This test shows the composition of gut microbes, so we can work on re-establishing a healthy balance of good bacteria in the gut.
Treating SIBO
SIBO treatment is often limited to the use of antibiotics and dietary restrictions (including avoiding FODMAPs, as explained later in this post). However, this treatment approach has severe limitations. Underlying causes of SIBO must be addressed, including these common causes:
- History of constipation, often stemming from a sluggish gallbladder
- Emotional stress, which impacts serotonin levels in the gut thus altering gut motility
- Chronic stress, which alters the response of the Vagus Nerve, impacting digestion
- Low stomach acid, which results in poor digestion of protein, allowing for putrefaction in the gut
- Sluggish gallbladder, which leads to poor digestion of fats
- Chronic infections (such as sinus and urinary tract infections) that increase dependence on antibiotics, which negatively impact gut health
- Use of proton pump inhibitors (PPIs) to reduce the production of stomach acid, a common treatment for acid reflux or gastroesophageal reflux disease (GERD), which can cause or contribute to SIBO
An effective SIBO treatment plan needs to address not only the bacterial overgrowth but also all the underlying causes of that overgrowth; for example:
- A sluggish gallbladder, far more common in women than in men, often goes undiagnosed because the problem is subclinical. In fact, the majority of women I see with gallbladder issues have no readily detectable medical findings associated with a gallbladder problem. It’s not until we perform a history and physical exam during our initial consultation that the problem is identified. The signs are vague — bloating after eating (similar in SIBO), feeling poorly after eating a fatty meal or fried food, experiencing shoulder pain (referred from the gallbladder), stomach pain, heartburn (often coming from poor gallbladder function), constipation, or loose stools (again like SIBO). Dietary changes and supplements can be used to restore gallbladder function.
- Improperly digested fats set the stage for bacterial overgrowth and inflammation in the digestive tract. Although carbs are often identified as the prime suspects behind SIBO because they feed bad bacteria in the gut, I have found clinically that fat digestion is just as important and often overlooked. Treatments to improve liver and gallbladder function along with short-term supplementation with pancreatic enzymes and long-term changes to diet can improve fat digestion.
- The Vagus Nerve can lose its tone when the brain is subjected to chronic stress. Think of tone in terms of tuning a musical instrument. The Vagus Nerve needs to be tuned to produce the proper tone for signaling digestion. When subjected to chronic stress, the brain signals for cortisol and adrenaline, which alters the tone of the Vagus Nerve over time leading to impaired digestion. There are exercises to stimulate the Vagus Nerve as well as nutrients to calm the mind, thereby restoring Vagus Nerve tone and function.
In each of these cases, treating the underlying cause of SIBO, in addition to reducing the microbial population in the small intestine, leads to a better long-term outcome.
Adopting a Low FODMAP Diet
FODMAPs are foods containing hard-to-digest carbohydrates and sugar alcohols. (FODMAP stands for Fermentable Oligo-, Di-, Mono-saccharides And Polyols.) The low FODMAP diet is typically used to treat IBS and other functional gastrointestinal disorders (FGIDs), but it is also very useful in SIBO treatment. Keep in mind, however, that diet is only one of the many possible contributing factors; all contributing factors must be addressed.
For many people with SIBO there a few trigger foods, so not all FODMAP foods need to be avoided or eliminated from the diet. In my experience, the most common trigger foods for SIBO are:
- Dairy
- Garlic
- Onions
Every person is different, so I work closely with my patients to identify their trigger foods and make targeted dietary adjustments.
The Low FODMAP Diet (from Monash University) is very restrictive. Here’s a list of the foods you can eat:
| Food group | Specific foods |
| Vegetables | Alfalfa, bean sprouts, green beans, bok choy, capsicum (bell pepper), carrot, chives, fresh herbs, choy sum, cucumber, lettuce, tomato, zucchini, and the green parts of leeks and spring onions |
| Fruits | Orange, grapes, and melon |
| Protein | Meats, fish, chicken, tofu (not silken), and tempeh |
| Dairy | Lactose-free milk, lactose-free yogurts, and hard cheese |
| Breads and cereals | Gluten-free bread and sourdough spelt bread, crisped rice, oats, gluten-free pasta, rice, and quinoa |
| Biscuits (cookies) and snacks | Gluten-free biscuits, rice cakes, and corn thins |
| Nuts and seeds | Almonds (no more than 10 nuts per serving) and pumpkin seeds (no cashews or pistachios) |
| Beverage options | Water, coffee, and tea |
Other sources confirm the suitability of these and suggest some additional foods.
Download the Monash University Low FODMAP Diet app for on-the-go support.
If you suspect that you may be suffering from SIBO, the first step is to find a doctor who fully understands all of the possible contributing factors and then schedule a visit for examination and testing. Effective treatment requires an accurate and thorough diagnosis that not only confirms (or rules out) SIBO but that identifies what’s causing it.
———-
Disclaimer: The information in this blog post is provided for general informational purposes only, and may not reflect current medical thinking or practices. No information contained in this post should be construed as medical advice from Dr. Matt Lewis, D.C., DACBN, CFMP®, nor is this post intended to be a substitute for medical counsel on any subject matter. No reader of this post should act or refrain from acting on the basis of any information included in, or accessible through, this post without seeking the appropriate medical advice on the particular facts and circumstances at issue from a licensed medical professional in the recipient’s state, country or other appropriate licensing jurisdiction.
———-
About the Author: Dr. Matt Lewis, D.C., DACBN, CFMP®, specializes in diagnosing and treating the underlying causes of the symptoms related to chronic and unexplained illness through nutrition, lifestyle, chiropractic, and other natural approaches to whole-health healing in Tampa, Florida. He earned his B.S. in Biology from Shenandoah University, his Doctorate in Chiropractic from Life University, his Diplomate status in Clinical Nutrition from the American Clinical Board of Nutrition, his CFMP® from Functional Medicine University, and his certification as a Digestive Health Specialist (DHS) through the Food Enzyme Institute. Dr. Lewis’ passion for health and wellness stems from his own personal experience. With a family history of autoimmune conditions and diabetes, and his own lab tests showing his genetic susceptibility to Hashimoto’s thyroiditis (autoimmune thyroid), he has learned how to restore his own health and vigor to prevent the onset of these and other illnesses and live an incredibly active life. Through this process, he acquired a deeper understanding of health and wellness, which he now offers his patients in Tampa.



Trying to find out about testing and treatment for SIBO and if you take my insurance which is Blue Cross Blue Shield PPO
did you take Ambetter insurance EPO ?