You may have recently read about the owner of a Tampa thyroid practice who agreed to pay $4 million to the Federal government to resolve allegations that he knowingly engaged in unlawful billing practices. The doctor, who shall remain nameless here but is easily identified by googling the situation I just described, was charged with violating the False Claims Act (a.k.a., the Lincoln Law), which imposes liability on those who defraud governmental programs. And while the Wesley Chapel physician in question clearly violated the law by overbilling the Federal government for the treatments he doled out, there’s nothing whatsoever false about the danger associated with an out of control thyroid!
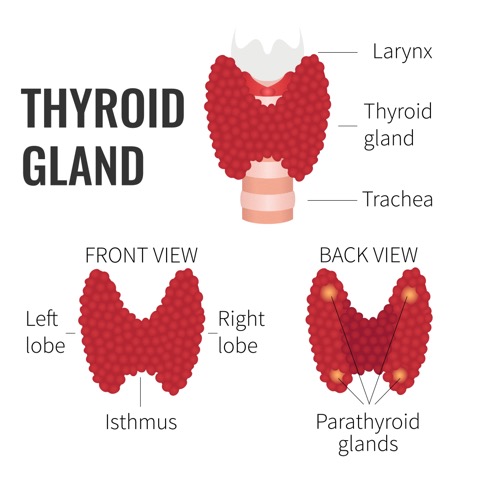
For the uninitiated, the thyroid gland controls metabolism, and every cell in the body requires adequate thyroid hormone to function properly. When the level of thyroid hormone is insufficient to support healthy function, the following symptoms commonly arise:
- Weight gain or resistance to weight loss
- Exhaustion
- Muscle pain
- Swelling
- Dry skin
- Poor digestion
- Brain fog
- Hair loss
- Irregular menstrual cycles
Common triggers of thyroid hormone include puberty, pregnancy, and peri-menopause. The condition is most common in women over the age of forty.
Hashimoto’s Thyroiditis
Most patients diagnosed with hypothyroidism have Hashimtoto’s thyroiditis, an autoimmune disorder (a condition in which the immune system attacks the thyroid). Patients who have Hashimoto’s thyroiditis are at an increased risk of developing other autoimmune disorders, including these:
- Type 1 diabetes mellitus: The body produces little or no insulin, or the insulin produced does not work as it should (insulin resistance).
- Graves’ disease: The thyroid produces too much thyroid hormone (hyperthyroidism).
- Rheumatoid arthritis: A chronic inflammatory condition affecting the joints, including those in the hands and feet.
- Pernicious anemia: The inability to absorb vitamin B12, potentially causing anemia and neurologic problems.
- Addison’s disease: Adrenal failure; the adrenal gland provides cortisol to handle stress and illness.
- Premature ovarian failure: Early menopause.
- Vitiligo: Patches where the skin loses its pigmentation.
- Thrombocytopenic purpura: A bleeding disorder due to inadequate platelets in the blood.
- Systemic lupus erythematosus (SLE): An autoimmune disease that can affect the skin, joints, heart, lungs, kidneys, and other organs.
Symptoms of hypothyroid and Hashimoto’s thyroiditis can start at any age and may persist even when a person is taking thyroid medication.
Conventional Medicine Diagnosis and Treatment
Practitioners of conventional medicine often test levels of thyroid stimulating hormone (TSH), T4 (thyroxin), and T3 (triiodothyronine), when they suspect hypothyroidism may be causing certain symptoms. However, they rarely test for Hashimoto’s thyroiditis, because the current health care system will not cover the cost of the test or because conventional treatment for it is the same for any cases of hypothyroidism, regardless of the cause.
Standard treatment involves monitoring thyroid hormone levels and prescribing hormone replacement with synthetic T4, T3, or both. Instead of synthetic T4, some doctors will prescribe a natural hormone derived from porcine (pig) thyroid, such as Naturethroid, Armor, or Westhroid.
Functional Medicine Diagnosis and Treatment
Functional medicine practitioners like myself take a different approach. Instead of merely providing what the thyroid is incapable of producing on its own, we want to know why the thyroid is not functioning properly, so we can take steps to restore proper function.
Because Hashimoto’s thyroiditis is at the root of nearly 90 percent of all cases of hypothyroidism, I first test to determine whether the body’s immune system is producing antibodies to the thyroid. If such antibodies are detected, I know that the cause of the hypothyroidism is an autoimmune disorder, not simply a thyroid disorder, and I treat the identifiable underlying causes of the autoimmune disorder.
Treatments often involve improving gut health, identifying food sensitivities and adjusting the diet accordingly, reducing stress, and increasing levels of physical activity. By restoring healthy immune function, I not only restore healthy thyroid function, but I also help my patients reduce the risk of developing other autoimmune disorders.
If testing rules out Hashimoto’s thyroiditis, I conduct additional tests to identify the cause(s). By assessing genetics, lifestyle, and dietary patterns and using a metabolic survey, I identify the various factors that are impacting thyroid health and function and tailor a treatment plan to address the underlying conditions. Treatment typically involves changes to diet and lifestyle along with supplements for improving overall thyroid health and function, but treatment varies considerably according to the underlying factors contributing to the thyroid dysfunction.
In autoimmune thyroid, the attack on the thyroid causes it to malfunction. The gland itself is being injured. However, the thyroid can malfunction for other reasons. Anything that blunts the ability of the thyroid to produce hormones can cause hypothyroid, including the following:
- Physical trauma in the cervical spine
- Various medications
- Pituitary dysfunction
- Chronic inflammation (typically from elevated blood sugars)
In the following sections, I discuss these possible causes in more detail.
Physical trauma
People can develop hypothyroid following a motor vehicle accident or whiplash injury. This may be due to a temporary inflammatory response and may self resolve on its own or continue for years.
Medications
A research review entitled “How medications affect thyroid function,” published in the Western Journal of Medicine, Betty J Dong concludes that “The accurate interpretation of abnormal thyroid function test results may be complicated by the concomitant presence of medications and nonthyroidal illnesses.”
In my experience, physicians are often aware of the various impacts that medications can have on thyroid health and treatment. However, the relationships of these medications to the patients experiencing symptoms are often overlooked or, because the medication is deemed necessary to treat another condition, the hypothyroid condition is approached as an unfortunate side effect and treated with thyroid hormone replacement.
Pituitary Dysfunction
The pituitary gland releases thyroid stimulating hormone (TSH) that signals the thyroid gland to produce T4 and T3. In some cases of hypothyroid, the primary issue is due to a slowing down of the pituitary gland. In such cases, while thyroid hormones are at low levels, it’s not the thyroid itself that is malfunctioning but the feedback mechanism that signals the thyroid to produce more T4 and T3. Instead of focusing exclusively on the thyroid, diagnosis needs to probe deeper to explore why the pituitary is not functioning as it should.
Chronic inflammation
Chronic inflammation resulting from elevated blood sugars, infections, or psychological stress can impact the ability of the hypothalamus to communicate with the pituitary gland causing hypothyroid.
Therefore, in some cases, balancing blood sugar is the key to regulating thyroid activity. This can be accomplished using various vitamins and minerals and paying close attention to diet and exercise. Often, patients are unaware of blood sugar issues because they have not had the proper tests run, including fasting insulin, c-peptide, HBA1C, and glucose levels. It’s not accurate to say your blood sugar is normal just because the glucose level is in the normal range. Fatigue after eating is often a sign that the various systems used to regulate blood sugar have been compromised.
Starting with the Right Diagnosis
Proper treatment of hypothyroid requires more than merely supplementing T4 and T3 when levels are low. An accurate diagnosis is necessary to determine why T4 and T3 levels are low and then treatment must address the underlying cause, whether it is Hashimoto’s thyroiditis, physical trauma, medications, pituitary dysfunction, or chronic inflammation.
Whether you see a conventional or functional medical doctor, keep in mind that diagnosis is the key to proper treatment, and make sure your doctor tests for thyroid antibodies to determine whether the cause of your hypothyroidism is an autoimmune disorder or something else. Until you know the cause, you are merely treating the symptoms.
The people I treat with symptoms of hypothyroid see vast changes in their quality of life, including weight loss, increased energy, more restful sleep, less pain, and clearer thinking.
– – – – – – – – – – –
About the Author: Dr. Matt Lewis, D.C., CFMP®, specializes in diagnosing and treating the underlying causes of the symptoms related to chronic and unexplained illness through nutrition, lifestyle, chiropractic, and other natural approaches to whole-health healing in Tampa, Florida. He earned his B.S. in Biology from Shenandoah University, his Doctorate in Chiropractic from Life University, his CFMP® from Functional Medicine University, and his certification as a Digestive Health Specialist (DHS) through the Food Enzyme Institute. Dr. Lewis’ passion for health and wellness stems from his own personal experience. With a family history of autoimmune conditions and diabetes, and his own lab tests showing his genetic susceptibility to Hashimoto’s thyroiditis (autoimmune thyroid), he has learned how to restore his own health and vigor to prevent the onset of these illnesses and live an incredibly active life. Through this process, he acquired a deeper understanding of health and wellness, which he now offers his patients in Tampa.



Leave A Comment